2025 Tufts Medicare Preferred
Access (PPO) Plan
- $1,500 Dental Flex Advantage Spending Card!
- $0 Medical Deductible
- Prescription Drug Coverage Included
- $185 Annual Wellness Allowance
- $250 Annual Eyewear Benefit
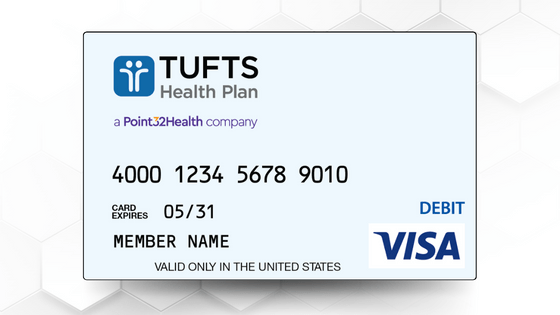
Flex Advantage Spending Card
The Flex Advantage spending card allows Tufts Health Plan Medicare Preferred Access (PPO) Plan members to see any dentist in the country who accepts Visa® — no network, cost sharing, or other restrictions to worry about. Learn more about the Flex Advantage spending card by clicking the link below.

Tier 1 Drug Costs
Deductible
Preferred Retail Pharmacy
Non-preferred Retail Pharmacy

Tier 2 Drug Costs
Deductible
Preferred Retail Pharmacy
Non-preferred Retail Pharmacy

Tier 3 Drug Costs
Deductible
Preferred Retail Pharmacy
Non-preferred Retail Pharmacy

Tier 4 Drug Costs
Deductible
Preferred Retail Pharmacy
Non-preferred Retail Pharmacy

Tier 5 Drug Costs
Deductible
Preferred Retail Pharmacy
Non-preferred Retail Pharmacy

Tier 6 Drug Costs
Deductible
Preferred Retail Pharmacy
Non-preferred Retail Pharmacy

Catastrophic Coverage Stage
Once you've spent 2,000 in out-of-pocket prescription costs you are in the Catastrophic Coverage Stage. If you reach the Catastrophic Coverage Stage, you pay nothing for covered Part D drugs and for excluded drugs that are covered under our enhanced benefit.

Covered Insulin Drugs
Part B: $35/month (Other Part B Drugs: up to 20% in-network/40% out-of-network)
Part D: Your copay for covered insulin will not exceed $35 per 30-day supply regardless of the drug tier. This means that your copay is the Tier 1, Tier 2, Tier 3, or Tier 4 copay, or $35 per 30-day supply, whichever is lower.

Out-of-Pocket Maximum
$5,400 for in-network costs; $9,500 for a combination of in and out-of-network costs. This is the most you will pay in a plan year for covered medical expenses.
Annual Physical Visit
Your Annual Physical visit will cost you $0 per visit in-network; $0 of cost out-of-network. You are covered for one Annual Physical each plan year.

Annual Wellness Visit
Your Annual Wellness visit will cost you $0 per visit in-network; $0 of cost out-of-network. You are covered for one Annual Wellness each plan year.
Primary Care Provider (PCP)
$0 per visit in-network; $0 per visit out-of-network per Primary Care Physician (PCP) visit.
Specialist Copay
$40 per visit in-network; $40 per visit out-of-network per Specialist visit.

Routine Vision Exam
$0 per visit in-network; $40 per visit out-of-network. You are covered for one Annual Routine Vision exam each plan year.

Routine Hearing Exam
$0 per visit in-network; $40 per visit out-of-network. You are covered for one Annual Routine Hearing exam each plan year.

Laboratory Services
$0 per day in-network; 45% of cost per service per day out-of-network. Copay will not apply in addition to office visit or urgent care copay. Prior Authorization may be required for in-network services.
X-Rays
$30 per day in-network; 45% of cost out-of-network. Copay will not apply in addition to office visit or urgent care copay. Prior Authorization may be required for in-network services.
Diagnostic Procedures
$30 per day in-network; 45% of cost out-of-network. Copay will not apply in addition to office visit or urgent care copay. Prior Authorization may be required for in-network services.
Diagnostic Radiology Services
Ultrasounds: $100 per day in-network; Others: $140 per day in-network. These services generally include computed tomography (CT) and magnetic resonance imaging (MRI). Out-of-network: 45% of cost. Prior Authorization may be required for in-network services.

Outpatient Surgery
In-network: Colonoscopies: $0; Other outpatient surgeries (Ambulatory Surgical Center, ASC): $290 per day; Other outpatient surgeries (Non-ASC): $390 per day - for Outpatient Services in-network.
Out-of-network: 45% of the cost. Prior Authorization may be required for in-network services.

Physical, Occupational, and Speech Therapy
$30 per visit in-network; 45% of cost out-of-network. Physical Therapy often helps in recovering from surgery or injury and can help manage long-term health issues like arthritis. Occupational Therapy helps develop, recover, and improve the skills needed for daily living and working after an injury or disability. Speech Therapy generally helps manage speech, language, communication and swallowing disorders. Prior authorization may be required.

Cardiovascular Screening
$0 per visit in-network; $0 of cost out-of-network. These screenings and tests help detect conditions that can lead to a heart attack or stroke.
Cancer Screening (Colorectal, Prostate, Breast)
$0 per service in-network; $0 of cost out-of-network. These screenings are aimed at detecting cancer before symptoms appear, when treatment is more effective.
Urgent Care
$45 per visit in-network or out-of-network. Urgently needed services are provided to treat a non-emergency, unforeseen medical illness, injury, or condition that requires immediate medical care. Urgent care copayment is NOT waived if admitted inpatient within 1 day.

Emergency Room Visits
Emergency Room visits cost $125 per visit worldwide, and there is no limit to the number of visits in a plan year. Copay waived if admitted to observation or inpatient within 1 day for the same condition.

Inpatient Hospital Coverage
In-Network: Days 1-5: $400 per day, $0 per day after day 5
Out-of-Network: 45% of cost. Prior Authorization may be required.

Ambulance Rides and Services
$350 per one-way trip for medically necessary Ambulance Services. Prior authorization may be required for non-emergency transportation. Includes worldwide emergency transportation coverage.

Acupuncture
$20 per visit in-network; $45 per visit out-of-network. Covers up to 12 visits in 90 days for members with chronic lower back pain. 8 additional visits covered for those demonstrating an improvement. No more than 20 visits administered annually. Additional acupuncture services are eligible for reimbursement under your Wellness Allowance.
Embedded Dental Visa Flex Advantage Spending Card
Access PPO members receive a yearly dental benefit amount of $1,500, which can be used to pay for any non-cosmetic and non-Medicare-covered dental procedure. The full amount is loaded onto your Flex Advantage spending card at the beginning of the year. Just swipe your Flex Advantage spending card to pay for covered dental services up to the annual limit at any dentist in the country who accepts Visa. The balance does not carry over, so try to use it all before the end of the year. *Restrictions apply. Refer to your Evidence of Coverage (EOC) for details.
Calendar Year Maximum
Not Included - Dental Covered Under Flex Advantage Spending Card
Individual Annual Deductible
Not Included - Dental Covered Under Flex Advantage Spending Card
Periodic Oral Evaluation
Not Included - Dental Covered Under Flex Advantage Spending Card
Comprehensive Oral Exam
Not Included - Dental Covered Under Flex Advantage Spending Card
Intra Oral Bitewing X-ray (X-rays of Crowns of Teeth)
Not Included - Dental Covered Under Flex Advantage Spending Card
Intra Oral X-ray - Entire Mouth (Panoramic & Full Mouth)
Not Included - Dental Covered Under Flex Advantage Spending Card
Single Tooth X-ray Images
Not Included - Dental Covered Under Flex Advantage Spending Card
Silver Fillings and White Fillings
Not Included - Dental Covered Under Flex Advantage Spending Card
Periodontal Cleaning
Not Included - Dental Covered Under Flex Advantage Spending Card
Telehealth
In-network: Medicare-covered services plus additional telehealth services. $0 copay for e-visits, virtual check-ins, and remote patient monitoring with your Primary Care Provider (PCP) or Specialist; for all other telehealth visits, copay is the same as corresponding in-person visit copay.
Out-of-network: Medicare-covered services only. Additional telehealth services not covered. Cost share is the same as corresponding in-person visit cost share.

Hearing Aid Benefit
You are eligible for up to 2 covered hearing aids per year, 1 aid per ear. To be covered, the hearing aids must be on the Hearing Care Solutions* formulary and must be purchased through Hearing Care Solutions: $250 copay for Standard level hearing aid; $475 copay for Superior level hearing aid; $650 copay for Advanced level hearing aid; $850 copay for Advanced Plus level hearing aid; $1,150 copay for Premier level hearing aid.
*Hearing Care Solutions will be rebranding as TruHearing, Inc as of January 1, 2026

Over the Counter (OTC)
$130 per calendar quarter to spend on Medicare approved health-related OTC items. Members receive quarterly credit on the Flex Advantage spending card to use towards covered OTC items at participating retailers and plan approved online stores. Unused quarterly balances do not rollover. You may also purchase OTC hearing aids using your OTC benefits.

Eyewear Benefit
Up to $250 per year for standard eyeglasses (prescription lenses, frames, or a combination of lenses and frames) and/or contact lenses purchased from any provider. Upgrades are covered. The annual allowance may be used to purchase upgrades for Medicare-covered and/or therapeutic eyewear as well as routine/corrective eyewear.
Weight Management Programs
$150 reimbursement per year for fees related to weight management programs like WeightWatchers and hospital-based programs.

Wellness Allowance
Choose how to stay fit with up to a $185 reimbursement for fees you pay toward joining a health club, fitness class (such as aerobics, Pilates, Tai Chi, or yoga), nutritional counseling sessions and other wellness programs like memory fitness activities. Also included are alternative therapies, massage therapy, fitness tracking devices, and heart rate monitors.
This is a Medicare Advantage plan, also known as Medicare Part C. It provides you with all of your Medicare Part A and B benefits, as well as additional coverage not included in Parts A and B. By paying a monthly premium, you gain consistent co-payments and deductibles and a yearly out-of-pocket spending maximum. Medicare Part D prescription drug coverage is also included as a part of this plan.
You must continue to pay your Medicare Part B premium. If you receive Social Security, Railroad Retirement Board (RRB) benefits, or Civil Service benefits, your Medicare Part B (Medical Insurance) premium is already automatically deducted from your benefit payment.
A PPO plan provides you the freedom to access any doctor and hospital, and you don't need referrals. A PPO plan is a good option if you travel often or want to keep a doctor that is outside of the network. Seeing doctors inside the network will generally have lower costs for services than seeing a doctor outside of the network.
The service area for this plan are: Bristol, Essex, Middlesex, Norfolk, Plymouth, Suffolk, Hampden, Hampshire or Worcester counties.